Abstract
Background: Patients (pts) with malignancies are at increased risk of morbidity and mortality from COVID-19. Among these pts, some of the higher case fatality ratios (CFR) reported are among pts with myeloid malignancies, ranging from 37 to 50% (Mehta V, Cancer Discov 2020; Ferrara F, Leukemia 2020). Levine Cancer Institute (LCI) has a robust hematologic malignancy and cellular therapy program that serves many pts with myeloid malignancies, seeing nearly 100 new diagnoses of acute myeloid leukemia per year. A strategy to mitigate risks associated with COVID-19 was established at LCI in partnership with Atrium Health's (AH) Hospital at Home (HAH). HAH was a system wide platform using telemedicine and home health services to assess and monitor COVID-19 + pts at high risk of complications. To augment HAH for our medically complex cancer pts, a virtual health navigation process involving expertise from across LCI, including a specialized nurse navigation team, was developed to rapidly identify LCI pts + for SARS-CoV-2, monitor them under physician supervision, and escalate care as needed with AH HAH. Along with the navigation platform, data-driven guidelines for detecting, monitoring, and managing LCI pts + for SARS-CoV-2 were swiftly employed across the extensive LCI network. Herein we report on the outcomes for LCI pts with myeloid malignancies + for SARS-CoV-2 and outline the employed risk mitigation strategies and their potential impact on these outcomes.
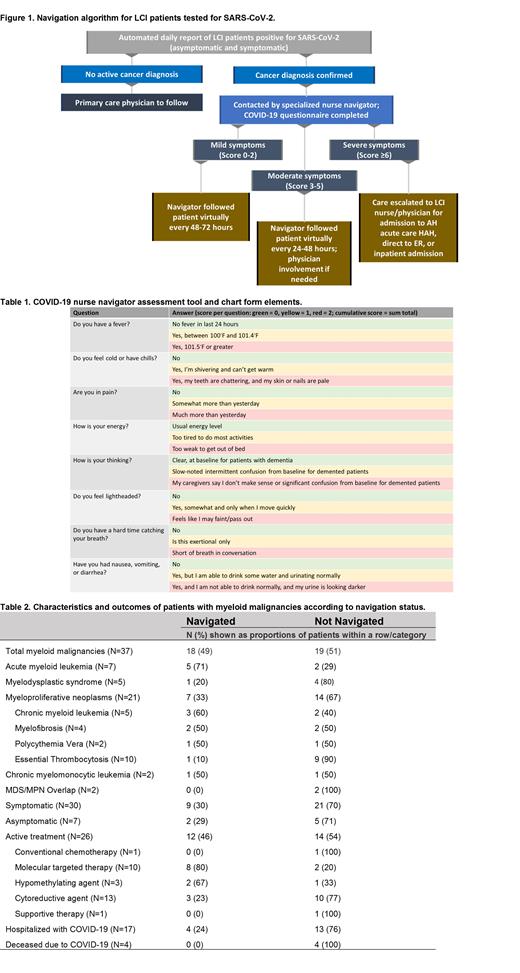
Methods: An automated daily list of LCI pts + for SARS-CoV-2 was provided by AH Information Services. Each pt's chart was reviewed by a nurse navigator for hematologic or oncologic diagnosis, outpatient or inpatient status, and COVID-19 symptoms. Pts without a cancer diagnosis were not assigned a navigator. If hospitalized, a pt was not assigned a navigator; following discharge, if enrolled in HAH, a navigator was assigned. In collaboration with HAH, an algorithm for directing care was utilized (Figure 1). A diagnosis-specific navigator contacted and screened the pt with an assessment tool, which scored pts for surveillance and treatment needs (Table 1). Documentation was forwarded to the primary hematologist/oncologist. Comprehensive guidelines for testing, scheduling, management of + pts, research, and process changes were created, disseminated, and actively updated through LCI's EAPathways. For outcome analysis for pts with myeloid malignancies, pt vital status was updated through data cutoff (7/3/21).
Results: From inception on 3/20/20 to 12/2/20, 974 LCI patients were identified as SARS-CoV-2 + and reviewed for nurse navigation. Of the 974 pts, including pts with benign and malignant diagnoses, 488 were navigated. Among all SARS-CoV-2 + LCI pts, 145 (15%) had a hematologic malignancy, including 37 (4%) pts with myeloid malignancies. Characteristics are shown in Table 2. Of the 37 pts, 18 (49%) were navigated. 70% with myeloid malignancies were on active treatment at the time of + test. Nearly 50% of those on active treatment were navigated. 46% were hospitalized with COVID-19, with this being the main reason for no assigned navigator. 24% of hospitalized pts were eventually assigned a navigator. Only 3 pts had undergone allogeneic stem cell transplantation (allo-SCT) with a median time from transplant to detection of SARS-CoV-2 of 9 months (range, 7-23). 2 out of 3 cases post allo-SCT were asymptomatic. No pt died from COVID-19 following allo-SCT. Among the navigated pts with myeloid malignancies, there was no death related to COVID-19. 4 pts, all of whom were hospitalized, died from COVID-19 (N=2, myelodysplastic syndrome with 1 on azacitidine; N=2, myeloproliferative neoplasm, both on hydrea). A CFR of 11% was demonstrated for LCI pts with myeloid malignancies.
Conclusions: A multidisciplinary response strategy liaising between AH HAH and LCI followed, assessed, and assisted cancer pts + for SARS-CoV-2. With our embedded nurse navigation team's specialized attention along with enhanced physician oversight and close collaboration with AH HAH, opportunities for care escalation or adjustments in cancer-focused care were promptly identified. In this setting, among the high-risk population of pts with myeloid malignancies, a lower CFR than has been reported was observed. A virtual navigation platform with HAH capabilities is a feasible, safe, and effective way to monitor and care for this high-risk population.
Moyo: Seattle Genetics: Consultancy. Chai: Cardinal Health: Membership on an entity's Board of Directors or advisory committees. Avalos: JUNO: Membership on an entity's Board of Directors or advisory committees. Grunwald: Amgen: Consultancy; Agios: Consultancy; Astellas: Consultancy; Daiichi Sankyo: Consultancy; Stemline: Consultancy; Bristol Myers Squibb: Consultancy; PRIME: Other; Trovagene: Consultancy; Blueprint Medicines: Consultancy; AbbVie: Consultancy; Med Learning Group: Other; Pfizer: Consultancy; Sierra Oncology: Consultancy; Janssen: Research Funding; Incyte: Consultancy, Research Funding; Gilead: Consultancy; MDEdge: Other; PER: Other; Cardinal Health: Consultancy; Karius: Consultancy. Copelan: Amgen: Consultancy.